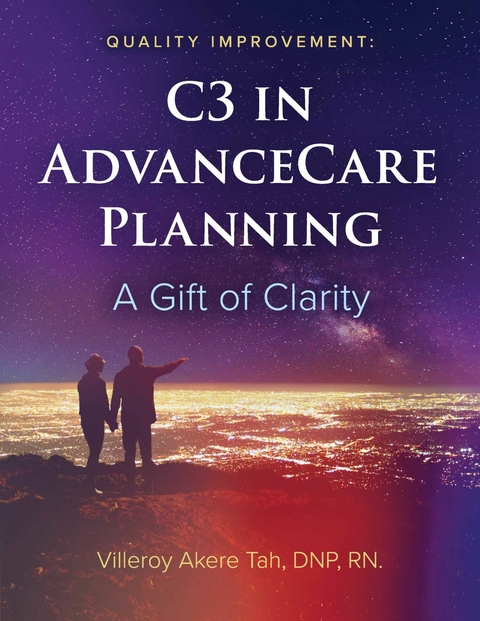
Quality Improvement: C3 in Advance Care Planning (eBook)
124 Seiten
Bookbaby (Verlag)
978-1-6678-3929-5 (ISBN)
The Collaborative Cultural Competence (C3) in Advance Care planning is a systems approach framework to tackle issues with low Advance Care Planning and Advance Directive completion in American adults and especially African Americans. The factors accounting for the continuous gap in AD completion among African Americans are not well understood. This book initiates the Advance Care Planning Conversation via a quality improvement project in a faith-based community. Collaboration at the micro and macro systems level is important between health care professionals in the acute and primary care settings, faith leaders, and health care providers in their communities. This approach allows patients to receive the care they need while in the community, rather than in an admitted hospital bed. This impactful book also offers the views and perspectives of some African Americans who have first-hand experience of the topic. The themes from these testimonials are key to identifying vital barriers and solutions specific to the African American population. It will take cultural sensitivity and competence for health care professionals to meet the patients where they are. It will take collaboration at the micro and macro levels to make sustainable changes that will close the care gap. The outcome is a gift of clarity for the patient, their family, and the health care professionals - a win-win.
Chapter 1:
Improving Readiness in ACP
Behaviors among African American Adults in the Community
Introduction
Advance directives are written statements by individuals on often standardized forms on which they express their wishes and preferences for treatment options should individuals become unable to make those decisions. Sixty-three percent (or 2 in 3) of American adults have not completed an AD (Yadav, Gabler, Cooney, Kent, Kim, Herst, Mante, Halpern, & Courtright, 2017). Huang, Neuheaus, and Chiong (2016) report White older adults (44.0 percent) are more likely to possess ADs than Hispanics (29%) and Black older adults (24%). Although there have been increased legislative and clinical efforts in the past decade to increase the completion of advance directives, extensive research findings continue to show a gap in ACP with Black American individuals.
Although this Doctor in Nursing Practice (DNP) student was unable to find ACP studies conducted exclusively among the African American population in the community setting, the findings from the vastly studied Black American population will help guide evidence used in this project. This scholarly project aims to improve the quality of end-of-life care amongst African Americans by assessing participants’ awareness and knowledge about ADs, and improving modifiable behaviors associated with readiness to complete AD. The behaviors include appointing an HCA, completing a living will or HCP, discussing wishes with loved ones and the physician.
Background
The factors that account for lower ACP amongst African Americans are more complex than often portrayed in the discussion. Laury, Greenle, and Meghani (2019) report that factors that affect African Americans’ end-of-life care beyond trust include lack of access to care, lower income and education levels, relationships, and quality of communication with health care providers. The author’s professional and personal experiences from bedside nursing and caring for a chronically ill parent have contributed to inquiries on the evidence related to the problem, possible interventions, and the best setting to achieve desired outcomes given the population involved.
Kwak and Harley (2005) reported that non-White ethnic groups generally lacked knowledge of ADs and were less likely to support it. ACP discussed when one’s health care has deteriorated at the end-of-life remains difficult for patients and health professionals. The planning process tends to involve task-oriented documentation of crucial preferences such as resuscitation and place of death rather than discussing the patient’s care goals (Pollock & Wilson, 2015). Koss and Baker (2017) report 40 percent of older adults in America become unable to make medical decisions at the end-of-life. The continuous progress with health care technologies in prolonging lives without necessarily improving quality of health, and the continuous gap in readiness for ACP, create the urgency for equitable health care and quality health care. When patients are admitted to the hospital in an acute or confused state without a pre-existing AD, there may be a delay in care (Carson & Bernacki, 2017). Further, the authors report health professionals understood the experiences that will take time to understand the patient’s baseline knowledge of their health and end-of-life preferences from family members if there is access to one. If the health care professionals cannot find any history or care preferences for the patient in documentation, they may intuitively choose to do everything possible to save the patient’s life. These decisions may be directed from individualized patient and family preferences. Sometimes, this may include a blood transfusion, an invasive surgical intervention, and resuscitation if the patient’s heart stops. Carson and Bernacki (2017) report that the lack of AD planning may result in emotional distress in bereaved families, moral distress with health professionals, and escalated non-coursed costs without accompanying measurable benefits to patients’ survival or quality of life end-of-life leave ethical confusion of what to do as the “right thing.”
Although impeding factors like diagnosis, spirituality, and poverty are not modifiable by the nurse, the nurse plays a vital role in collaboration with health care and community partners to break barriers associated with the persistent gap in ACP decisions. For example, a stakeholder revealed that many people “shy” away from ACP conversations; they put it off later when they become sick because of uncertainties regarding the process and prioritize other stressful and more pressing things faced with often (personal communication, 2021). This procrastination partly explains why readiness for ACP may be lower in non-White or minority communities often dealing with different types of social and economic stressors. Building confidence with advance planning conversation is a juxtaposition based upon a voluntary discussion versus one that needed to occur to honor one’s wishes during declining health prognosis.
Significance
Literature reports readiness for engagement in ACP follows expected behaviors reported in the process of AD completion and ACP itself (Fried, Redding, Robbins, Paiva, O’Leary, & Iannone, 2010). They said that these behaviors include completing a living will, HCP, communicating health care treatment preferences, perception of quantity versus quality of life with loved ones, and sharing these issues with the physician. The authors further report readiness is a process that occurs in stages and is affected by factors such as the individuals’ values and understanding of what ACP means. Therefore, understanding the barriers to readiness for ACP will be helpful when proposing meaningful interventions to increase the completion of AD.
In a customer discovery process in a faith-based setting and as reported from initial interactions with the congregants on the topic of ACP, the DNP student determined a need to address the practice community gap based on non-compliance and knowledge of AD. The initial assessment data informed the project on impactful interventions that will meet the needs of the congregants based upon trust and the accurate information to make life-sustaining personal decisions. The hope is that individuals express improvement in any ACP behaviors (appoint an HCA, discuss wishes with loved ones and physicians, complete an HCP form) before the end of the project.
Problem Statement
Health and health care disparity among minority ethnic groups, especially African Americans, is a social and public health crisis that warrants mentioning when discussing the completion of AD. Furthermore, the combined impact of the Covid-19 pandemic, which disproportionately affected the Black individuals, and the police brutality against a Black American (Floyd, 2020), again exposed the effect of systemic racism on the well-being of African Americans. This project addresses equitable access to quality health care, and expert health care end-of-life discussion with licensed nursing professionals and their population (African American adults participants) was intended to improve ACP behaviors. The behaviors encompass making preferences known to loved ones and physicians and completing an AD.
Concepts and Definitions
ADs are treatment preferences and the designation of a surrogate decision-maker if an individual becomes incompetent to make medical decisions on their behalf, and AD may be categorized into three types, namely living will, power of attorney, and HCP (Davis, 2021). With the durable power of attorney for health care, the individual nominates one or more persons who will communicate their wishes or preferences should they become incapacitated.
A living will is a written statement that specifies the types of medical treatments an individual desires (Davis, 2021).
HCP is a legal document in which individuals select someone trustworthy to make health care decisions if they become incapable of making their wishes known (Davis, 2021).
Readiness describes the level of preparedness on one end of the spectrum (pre-contemplation phase) to contemplation, to taking action and to the other end, maintaining action on engaging in ACP. It should be noted that “readiness is not a linear process.” This project focused on improving participants’ behavior to identify and designate an HCA and to complete an HCP if possible.
PICOT Question
The purpose of this quality project is to seek an answer to the inquiry. Among African American congregants at a Christian Church in a suburban city in Massachusetts (P), is a multi-modal intervention (to include educational videos, print medium, and live discussions with participants) on advanced care planning (ACP) (I), over three months (T), associated with an increase in knowledge of ACP and readiness to identify an HCA and complete of Health Care Proxy (HCP) (O)?
Purpose Statement
Evidence suggests lower rates of ACP are associated with adverse health outcomes at end-of-life. Readiness in this project is the willingness to do something among the congregants. The ACP behaviors are the characteristic response identified in prior studies to complete an AD. They include appointing an HCA, informing family and physicians on choices and preferences, and completing an HCP. Improving ACP behaviors among the church-based participants may increase ACP and, as a result, improve rates of their AD completion and, subsequently, the cost of health...
| Erscheint lt. Verlag | 1.5.2022 |
|---|---|
| Sprache | englisch |
| Themenwelt | Sachbuch/Ratgeber ► Gesundheit / Leben / Psychologie |
| ISBN-10 | 1-6678-3929-2 / 1667839292 |
| ISBN-13 | 978-1-6678-3929-5 / 9781667839295 |
| Haben Sie eine Frage zum Produkt? |
Größe: 6,8 MB
Digital Rights Management: ohne DRM
Dieses eBook enthält kein DRM oder Kopierschutz. Eine Weitergabe an Dritte ist jedoch rechtlich nicht zulässig, weil Sie beim Kauf nur die Rechte an der persönlichen Nutzung erwerben.
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen dafür die kostenlose Software Adobe Digital Editions.
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen dafür eine kostenlose App.
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich