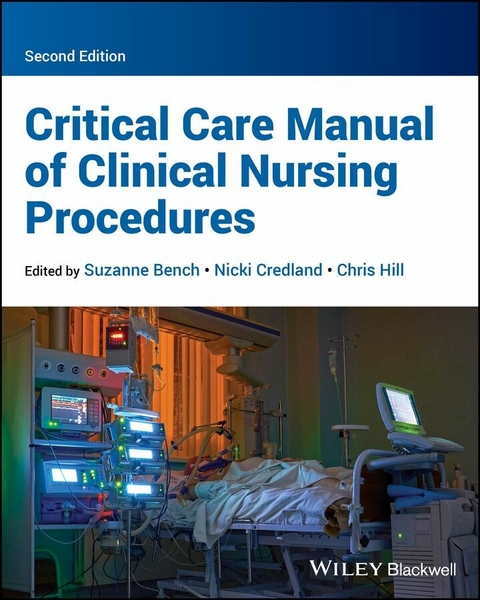
Critical Care Manual of Clinical Nursing Procedures (eBook)
688 Seiten
Wiley-Blackwell (Verlag)
978-1-119-84125-8 (ISBN)
Critical Care Manual of Clinical Nursing Procedures
The second edition of Critical Care Manual of Clinical Nursing Procedures is a practical overview of essential procedures for the care of critically ill patients. Beginning with chapters outlining the current scope of critical care, the book adopts a systematic stage-by-stage approach from admission to discharge. At each stage, it provides insights into physiology, key procedures, and the relevant evidence base. Now fully updated to incorporate the latest research and best practices, this volume is poised to remain an indispensable resource for the next generation of critical care providers.
Readers of the second edition will find:
- In-depth, beat-by-beat analysis of key procedures in critical care
- Interventions underpinned by the latest evidence
- Content aligned with the National Critical Care Competency Framework and endorsed by the British Association of Critical Care Nurses
Critical Care Manual of Clinical Nursing Procedures is ideal for nurses working in a critical care unit, nurses undertaking post-qualification specialist courses in critical care, or other healthcare professionals working as part of a critical care team.
Suzanne Bench is Director of Nursing for a centre of research for nurses and midwives at Guys and St Thomas NHS Trust and Professor of Critical Care Nursing at London South Bank University, as well as honorary Senior Lecturer at King's College, London, UK. She is an experienced clinical-academic intensive care nurse who sits on the executive board of the British Association of Critical Care Nurses.
Nicki Credland is a Reader in Critical Care at the University of Hull and a qualified and experienced critical care nurse. She was Chair of BACCN throughout the Covid-19 pandemic and advises NHS England on critical care nursing.
Chris Hill is a senior clinical practice educator at the Royal Free Hospital, Hampstead, and a Senior Lecturer at Brunel University, London, UK. He leads an Intensive Nursing Care course at the Royal Free for ICUs in North Central London and other parts of the capital.
CHAPTER 1
Scope and Delivery of Evidence‐Based Care
Suzanne Bench1, Nicki Credland2, and Chris Hill3
1 Director of Nursing (Research) Guy’s and St Thomas’ NHS Trust and Professor of Critical Care Nursing London South Bank University, London, UK
2 Reader in Critical Care, University of Hull, Hull, UK
3 Senior Clinical Practice Educator, Royal Free London NHS FT and Senior Lecturer, Brunel University London, UK
AIMS AND CHAPTER OVERVIEW
About 200,000 people per year in the UK require critical care for many different reasons, ranging from acute medical emergencies, to major trauma incidents such as serious road accidents (Batchelor, 2021). People who develop a critical illness and their families deserve the best treatment and care that can be provided, to optimise their health outcomes, experiences and quality of life. Excellence, however, requires appropriate interventions with a strong evidence base and practitioners1 who are competent to deliver treatment and care. The aim of Critical Care Manual of Clinical Nursing Procedures, 2nd edition is to detail the latest research and rationale for evidence‐based procedures and competencies related to the provision of adult critical care. As such, the manual is ideally placed to be used as a reference and resource for advancing critical care practice and education for nurses and the wider multi‐professional team. This chapter describes how critical illness needs are classified, provides an overview of key national policies and discusses the role of the manual in the introduction of evidence‐based practice. Whilst mainly focused on the context of critical care nursing within the United Kingdom (UK), the content is relevant to critical care practitioners worldwide.
BACKGROUND AND CLASSIFICATION OF CRITICAL ILLNESS AND CRITICAL CARE IN THE UK
Critical care is defined as a ‘multi‐professional, multidisciplinary service which must deliver an integrated care pathway focused on patient need whilst addressing quality, governance and supporting optimal outcomes for patients’ (NHSE, 2022).
‘Critical care’ is an umbrella term encompassing both intensive and high dependency care for adults. Critical care provision has developed considerably over many years. A defining moment was publication of the Department of Health policy document entitled ‘Comprehensive Critical Care’ (Department of Health, 2000). This strategy document led to a restructure of the organisation of critical care services by advocating that provision of care should extend beyond the walls of an intensive care unit (ICU). It set out the vision for how critical care should be delivered, replacing the division of intensive care and high dependency beds with a classification system focused on levels of care. Whilst the original classification has since been updated (Table 1.1), the principle remains.
As in the original publication by the Department of Health (2000) and the 2009 Levels of Care document published by the Intensive Care Society (ICS), the 2021 Levels of Adult Critical Care (ICS, 2021) describes the care a patient requires, based on need. It merges the original level 0 and level 1 categories into one for people requiring ward level care, enabling ‘level 1’ to represent the need for Enhanced Care, and levels 2 and 3 the need for critical care. Levels 2 and 3 have also been amended to reflect contemporary needs of critically unwell people.
Table 1.1 Levels of adult critical care (Intensive Care Society (ICS), 2021 / with permission from Intensive Care Society)
| Classification | Definition |
|---|
| Ward Care |
|
| Level 1 Enhanced Care |
|
| Level 2 Critical Care |
|
| Level 3 Critical Care |
|
The organisation of care for different categories of need varies according to patient requirements and how this is accommodated by the local service. Adults with level 3 needs are generally cared for in a clinical area that is designated primarily for this category of patient and is often referred to as an intensive care unit (ICU). This is because this group need high levels of monitoring, intervention and organ support, which requires specialist expertise and equipment. Sometimes the level 3 care facility is also a ‘specialty only’ unit (such as patients with neurological problems or burns).
Patients defined as requiring level 2 or level 1 support are cared for in a wider variety of settings, with an increase in the number of enhanced care beds currently being developed. Settings include designated units (which may or may not include specialist‐only beds); specific area/beds within a level 3 facility (which may or may not include specialist‐only beds); and specific area/beds within a ward level care facility (which may or may not include specialist‐only beds). Patients cared for in a ward‐based facility are often there on a temporary basis with the support of the multidisciplinary critical care outreach team.
While the levels of critical care are clearly defined, allowing for a joint understanding of the needs of patients and the required level of care, a variety of designations and terms have been used to describe critical care facilities; these include intensive therapy (or care) unit (ITU or ICU), critical care unit (CCU), high dependency unit (HDU), special care unit (SCU) and post‐anaesthetic care unit (PACU). It is important, therefore, that the patient’s needs and the care facility are clearly and accurately identified and that all involved in service planning and provision and delivery of care have a shared understanding to effectively and efficiently meet the patient’s requirements. For the purposes of this manual the term ‘critical care’ refers to patients requiring care at levels 2–3, whereas ‘enhanced care’ refers to patients requiring level 1 care.
As well as the varying levels of critical care required and the locations where this care can be delivered, the characteristics of the patient population are important in determining the level of care required.
The varying patient characteristics and the complexity of caring for the critically ill...
| Erscheint lt. Verlag | 30.10.2024 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Pflege |
| Schlagworte | clinical nursing procedures • competency-based practice • critical care admission • critical care discharge • end of life care • Evidence-based Nursing • National Health Service • NHS • Patient Care • patient family care • Physiology |
| ISBN-10 | 1-119-84125-9 / 1119841259 |
| ISBN-13 | 978-1-119-84125-8 / 9781119841258 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Größe: 25,8 MB
Kopierschutz: Adobe-DRM
Adobe-DRM ist ein Kopierschutz, der das eBook vor Mißbrauch schützen soll. Dabei wird das eBook bereits beim Download auf Ihre persönliche Adobe-ID autorisiert. Lesen können Sie das eBook dann nur auf den Geräten, welche ebenfalls auf Ihre Adobe-ID registriert sind.
Details zum Adobe-DRM
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen eine
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen eine
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich