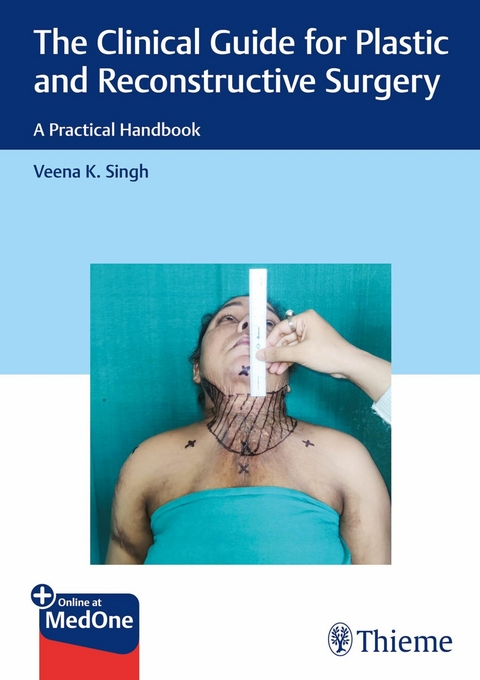
The Clinical Guide for Plastic and Reconstructive Surgery (eBook)
845 Seiten
Thieme Medical Publishers (Verlag)
978-81-966914-3-1 (ISBN)
The Clinical Guide for Plastic and Reconstructive Surgery: A Practical Handbook offers to resident doctors and consultants a unique compilation of comprehensive and authenticated information in a format that would help them prepare for practical examinations as well as in treating cases successfully. To mirror the practical exam format, the content of its 23 chapters, comprising 5 long and 18 short cases, is structured as questions and answers. In addition, for easy grasp and retention by the readers, the content follows a specific chronological sequence in delineating each case: history, general and local examination, investigations, how to proceed, stepwise planning, and surgical procedures.Salient Features:Learning objectives at the beginning of each chapter enhance the content and help align a reader's thought process better.Photographs and illustrations depict every step of clinical examinations and surgical markings; flowcharts and algorithms depict the line of management.Covers questions posed to plastic surgery residents in examinations and viva voce.
| 1 | Lower Leg Defect with Exposed Bonep Veena K. Singh |
Learning Objectives
At the end of this chapter, the students will be able to:
1.Understand the anatomy of lower leg.
2.Describe the clinical presentation of a case of lower leg wound.
3.Demonstrate the motor and sensory examination of lower extremity.
4.Understand the approach to a lower limb injury.
5.Perform the appropriate flap reconstruction for coverage of leg wound.
Introduction
The management of lower limb wound starts with a thorough examination of the wound and leg both. The primary goal of reconstruction is the restoration of functionality. It includes not only a stable skeletal base but also robust surrounding soft tissues like muscles, neurovascular structures, and skin envelope. A very good understanding of the tissue loss and its replacement with like tissues along with prevention of chronic pain and wound infection are important key aspects for a successful outcome.
Chief Complaints of the Patient
•Wound over the lower leg.
•Inability to bear weight on the affected limb.
•Pain/Discharge from the wound.
•Restricted movements of the joints.
History of Present Illness
1.Duration of injury/leg defect/exposed bone/wound.
2.Mode of injury including velocity of the vehicle in case of road traffic accident (RTA).
3.Immediately, what happened after the accident:
•Bleeding.
•Dangling of limb.
•Loss of consciousness/ear/nose bleed/vomiting.
•Unable to move limb.
•Condition of wound:
–Bone/Fracture—visible/not visible.
–Skin flaps avulsed/not visible.
•Whether immediate splintage at injury site.
•Associated trauma:
–Vertebral fracture
–Maxillofacial fracture
4.Primary aid was given/not given—Where and What?
•Debridement of wound.
•Application of plaster of Paris (PoP) slab/cast.
•Blood transfusion received, if any.
•Application of external fixator.
•Condition of wound after external fixator.
•Seen by plastic surgeon team/not (if yes—what advice/intervention).
•Type and frequency of dressing.
•Management of associated injury, if any.
5.Referral to plastic surgery after how many days.
•What was the condition of wound as told by treating doctor?
•What was the advice given?
•Any intervention done at that time?
6.Associated pain/fever/inability to move the foot.
7.Bladder/Bowel function.
8.Sleep/Appetite.
Past History
History of diabetes, hypertension, tuberculosis, any other medical illness, and history of any surgery done in the past.
Personal History
Married/unmarried, number of children, socioeconomic status, diet, history of smoking/alcohol intake, tobacco chewing. Alcohol intake history would include whether a regular/occasional drinker, and amount on daily basis if a habitual drinker. Smoking history must include the no. of cigarettes/bidis pack per day and number in each pack. The detailed history will give an idea about the ischemic effects of nicotine if a pedicled flap is planned for coverage of the defect. Alcohol intake will provide information about the general status of the patient.
Family History
Parents—whether elderly and dependent, siblings.
History of Allergy
To any specific food or medicine.
Treatment History
Any intervention for fracture stabilization, history of blood transfusion, history of injection Penicillin.
General Physical Examination
•Conscious level.
•General temperature (one should have a thermometer).
•Build.
•Nutrition.
•Pallor/cyanosis/jaundice/clubbing/edema.
•Pulse/BP (must)/respiration.
•Neck veins/glands.
•General condition of skin.
Systemic Examination
Local Examination
Take proper informed consent and examine the patient in adequate light.
Exposure
•Both limbs from the anterior superior iliac spine (ASIS) to the toes.
•Private areas need to be covered.
Important: If patient is ambulatory, observe the gait (if foot drop is present, then the cause must be looked for and also the level of nerve injury).
Inspection
1.Attitude and apparent shortening, if any.
2.Atrophy/Wasting—over thigh, leg, foot; always compare with the normal limb.
3.External fixator—extent and type of fixator needs to be described.
4.Pin tracts—granulation tissue/pus discharge, if any.
5.Wound (Fig. 1.1):
Fig. 1.1 Lower leg defect with exposed bone with external fixator in situ
•Site in terms of distance from anatomical landmarks.
–Proximally: Lower end of patella, medial/lateral femoral condyle.
–Distally: Lateral/medial malleoli.
–Medially: Anterior tibial border.
–Laterally: Posterior midline.
•Size: In longitudinal and transverse dimensions (approximately in cm).
•Margins: Whether epithelialization present or not.
•Granulation tissue: Fine/coarse, pink/beefy red, bleeds easily on touch or not so as to differentiate between healthy and unhealthy granulation tissue.
•Slough: Any visible dead and necrotic tissue.
•Discharge: Whether Yes/No. If yes, then amount, color, odor, consistency, from which part of wound.
6.Exposed Bone:
•Site: For example, patella/femoral condyles, upper/middle/lower third of tibia, ankle, malleoli, dorsum/sole of foot.
•Size.
•Fracture site and fragments: Visible/not visible.
•Alignment of the fracture fragments.
•Whether periosteum is intact.
•Appearance of the exposed bone:
–Living bone: Ivory white, shiny.
–Dead bone: Lusterless, yellowish, blackish.
•Whether anterior cortex/both cortex visible.
•Any exposed hardware.
7.Surrounding skin:
•Presence of multiple scars, hypopigmentation.
•Corn/Callosities.
8.Joint above and below: Condition of the skin, any swelling.
9.Foot: Condition of the skin: Whether dry, flaky.
•Look for signs of ischemia: Shiny/stretched, hair present or not.
•Pedal edema: Pitting or nonpitting.
Palpation
1.Temperature: As compared with the other limb or normal part of the same limb.
2.Tenderness: At the wound site and at edges.
3.Findings of the inspection of the are then corroborated.
4.Palpate for the peripheral pulses (in a trauma case, be careful of a single-vessel limb).
•Dorsalis pedis artery (DPA) in the space between the first and the second metatarsals.
•Posterior tibial artery (PTA): Between the posterior border of medial malleolus and tendoachilles.
•Popliteal artery: Palpated in the popliteal fossa.
5.Sensations: In territory of all cutaneous nerves and grade it according to the Medical
Research Council (MRC) scale.
•Over thigh and leg.
•Over foot—dorsum, first web space, sole, lateral and medial borders.
•Wound edges.
Movements
The active and passive range of movements at all joints of the lower limb must be checked and mentioned during the clinical examination.
1.Hip joint: Flexion, extension, abduction, and adduction.
2.Knee: Flexion and extension.
3.Ankle:
•Dorsiflexion and Plantarflexion.
–Subtalar joint (talocalcaneal) joint.
•Eversion/abduction and Inversion/adduction.
–Talocalcaneonavicular joint.
Measurements (After Squaring of Pelvis) (Fig. 1.2a, b)
Fig. 1.2 (a, b) Measurement of apparent and true shortening in a leg.
1.Total limb length:
•Keep the measuring tape from greater trochanter up to lateral malleolus.
•To be measured on both affected and normal sides.
•This gives the apparent shortening of the affected limb if it exists.
2.Leg:
•The length is measured from medial joint line to tip of medial malleolus.
•To be measured on both affected and normal sides.
•This gives the...
| Erscheint lt. Verlag | 7.8.2024 |
|---|---|
| Sprache | englisch |
| Themenwelt | Medizinische Fachgebiete ► Chirurgie ► Ästhetische und Plastische Chirurgie |
| Schlagworte | Plastic Surgery Cases • Plastic Surgery Exit Exam Preparation • Plastic Surgery Practical Exams • Plastic Surgery Residency Exams • Reconstructive Surgery |
| ISBN-10 | 81-966914-3-2 / 8196691432 |
| ISBN-13 | 978-81-966914-3-1 / 9788196691431 |
| Haben Sie eine Frage zum Produkt? |
Größe: 64,9 MB
DRM: Digitales Wasserzeichen
Dieses eBook enthält ein digitales Wasserzeichen und ist damit für Sie personalisiert. Bei einer missbräuchlichen Weitergabe des eBooks an Dritte ist eine Rückverfolgung an die Quelle möglich.
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen dafür die kostenlose Software Adobe Digital Editions.
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen dafür eine kostenlose App.
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich