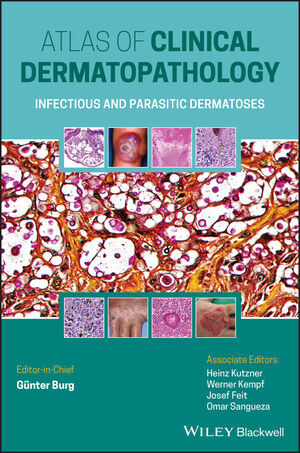
Atlas of Clinical Dermatopathology
Wiley-Blackwell (Verlag)
978-1-119-64706-5 (ISBN)
The »Atlas of Clinical Dermatopathology: Infectious and Parasitic Dermatoses« includes:
- A straightforward, pattern-based approach to dermatologic diagnosis
- full-color illustrations and clear descriptions for easy reference
- Combined clinical and histopathological perspectives
- Handy diagnostic tips throughout
Featuring all this and more, this invaluable atlas offers a uniquely balanced, clear, and comprehensive guide to what can be a difficult process, and will be of tremendous assistance to students, dermatologists, dermatopathologists, and pathologists everywhere.
Gunter Burg, MD, is Professor of Dermatology and Chairman Emeritus, University of Zurich, Zurich, Switzerland.
Heinz Kutzner, MD, is Professor of Dermatology, Institute of Dermatopathology, Friedrichshafen, Germany.
Werner Kempf, MD, is Professor of Dermatology, Department of Dermatology, University of Zurich, Zurich, Switzerland, and Founder and Co-Director of the dermatopathology laboratory Kempf und Pfaltz Histologische Diagnostik, Zurich, Switzerland.
Josef Feit, MD, is Associate Professor of Pathology, University of Ostrava, Ostrava, Czech Republic.
Omar Sangueza, MD, is Professor of Pathology and Dermatology, Director of Dermatopathology, Wake Forest School of Medicine, Winston-Salem, NC, USA.
1 Bacterial Infections 4
1.1. Staphylococcal and Streptococcal Infections. 4
1.1.1 Impetigo Contagiosa. 4
1.1.2 Ostiofolliculitis (Bockardt). 5
1.1.3 Pseudomonas (Gram Negative) Folliculitis (Whirlpool/Hot-Tub-Dermatitis) 5
1.1.4 Perianal Streptococcal Dermatitis. 5
1.1.5 Differential Diagnosis: Acne Papulopustulosa 6
1.1.6 Differential Diagnosis: Pseudofolliculitis Barbae 6
1.1.7 Ecthyma Gangrenosum 6
1.1.8 Abscess. 7
1.1.9 Furuncle 7
1.1.10 Carbuncle 7
1.1.11 Erysipelas (Cellulitis). 8
1.1.12 Phlegmon 8
1.1.13 Necrotising Fasciitis (Streptococcal Gangrene) *. 8
1.1.14 Hidradenitis Suppurativa (Acne Inversa) 9
1.2 Other Bacterial Infections: Corynebacteria. 9
1.2.1 Erythrasma 9
1.2.2 Pitted Keratolysis (Keratoma Sulcatum) 9
1.2.3 Trichobacteriosis (Trichomycosis) Palmellina 9
1.2.4 Erysipeloid 10
1.2.5 Anthrax. 10
1.2.6 Nocardiosis**. 11
1.2.7 Rhinoscleroma 11
1.3 Rochalimaea/Bartonellae. 11
1.3.1 Bacillary Angiomatosis and Cat Scratch Disease. 12
1.3.2 Verruga Peruana 12
1.3.3 Differential Diagnosis: Botryomycosis (Granuloma Pyogenicum; Lobular Capillary Hemangioma) 13
1.4 Mycobacterial Infections 13
1.4.1 Tuberculosis Cutis 13
1.4.1.1 Primary Tuberculosis of the Skin 14
1.4.1.2 BCG Vaccination Granuloma 14
1.4.1.3 Differential Diagnosis: Lupus Miliaris Disseminatus Faciei (LMDF) 14
1.4.1.4 Lupus vulgaris (LV) 15
1.4.1.5 Variant: Tuberculosis (Lupus) Cutis Verrucosa 15
1.4.1.6 Variant: Tuberculosis Cutis Colliquativa (Scrofuloderma). 15
1.4.1.7 Lichen Scrofulosorum (Tuberculosis Cutis Lichenoides). 16
1.4.1.8 Papulonecrotic Tuberculid 16
1.4.1.9 Erythema Induratum Bazin (EIB). 17
1.4.2 Atypical Mycobacteriosis: Fish Tank (Swimming Pool) Granuloma. 17
1.4.3 Leprosy (Hansen Disease) 18
1.4.3.1 Tuberculoid Leprosy. 18
1.4.3.2 Borderline Leprosy 19
1.4.3.3 Lepromatous Leprosy 19
1.4.3.4 Variant: Histoid Leprosy (HL). 19
1.4.3.5 Variant: Erythema nodosum leprosum (ENL) 20
1.4.4 Buruli Ulcer 20
1.5 Actinomycosis. 21
1.6 Borrelia Infections (Lyme Disease) 21
1.6.1 Variant: Erythema (Chronicum) Migrans (ECM) (Stage I) 22
1.6.2 Variant: Lymphadenosis Cutis Benigna (Pseudolymphoma, Lymphocytoma Cutis) (Stage I) 22
1.6.3 Variant: Morphea/Scleroderma-Like Lesions (Stage II) 24
1.6.4 Variant: Acrodermatitis Chronica Atrophicans (Stage III). 24
1.6.5 Variant: Juxtaarticular Fibrous Nodules in Acrodermatitis Chronica Atrophicans (Stage III). 25
1.6.6 Differential Diagnosis: Actinic Reticuloid* 25
1.7 Venereal Diseases 26
1.7.1 Gonorrhoea. 26
1.7.2 Syphilis, Chancre 26
1.7.2.1 Stage I. 26
1.7.2.2 Stage II 27
1.7.2.3 Stage III* 27
1.7.3 Ulcus Molle (Chancroid) 28
1.7.4 Granuloma inguinale (Donovanosis; Granuloma venereum) 28
1.7.5 Lymphogranuloma inguinale (lymphogranuloma venereum; Duran-Nicolas-Favre disease) 28
1.8 Rickettsial Infections. 29
1.9 Dermatoses Associated with Bacterial Infections 29
1.9.1 Staphylococcal Scalded Skin Syndrome (SSSS) 29
1.9.2 Differential Diagnosis: Toxic Epidermal Necrolysis (TEN) 30
1.10 Dermatoses Mimicking Bacterial Infections 30
1.10.1 Pyoderma Gangrenosum (PG) 30
1.10.2 Infantile Acropustulosis 31
1.10.3 Acute Generalized Exanthematous Pustulosis (AGEP) 31
1.10.4 Psoriasis Pustulosa 32
1.10.5 Localized Neutrophilic Eccrine Hidradenitis Associated with Mitoxantrone Treatment 32
1.10.6 Erosive Pustular Dermatitis (Pustular Ulcerative Dermatosis) of the Scalp. 33
2 Fungal Infections 33
2.1 Superficial Cutaneous Fungal Infections. 33
2.1.1 Variants: Tinea Corporis; Tinea Faciei. 34
2.1.2 Variants: Tinea Barbae; Tinea Capitis (Trichophytia) 34
2.1.3 Granuloma Trichophyticum (Majocchi’s Granuloma) 35
2.1.4 Candidiasis (Moniliasis). 35
2.1.5 Candida Tropicalis and Candida Lipolytica 36
2.1.6 Pityriasis (Tinea) Versicolor. 36
2.1.7 Variant: Malassezia (Pityrosporum) Folliculitis. 36
2.1.8 Differential Diagnosis: Seborrheic dermatitis 37
2.1.9 Tinea Nigra. 37
2.1.10 Piedra (Trichmycosis nodosa alba and nigra)*. 37
2.2 Subcutaneous Mycoses. 37
2.2.1 Sporotrichosis. 37
2.2.2 Mycetoma (Madura Foot). 38
2.2.3 Chromo(blasto)mycosis (Dermatitis Verrucosa) 38
2.3 Systemic Mycoses (Deep Fungal Infections) 39
2.3.1 Cryptococcosis (Torulosis, European Blastomycosis) 39
2.3.2 North American Blastomycosis (Blastomycosis, Chicago Disease). 40
2.3.3 Lobomycosis (Lobo Disease, Keloidal Blastomycosis, Blastomycoid Granuloma). 41
2.3.4 Histoplasmosis 41
2.3.5 Coccidioidomycosis (Desert or Valley Fever, San Joaquin Fever) 41
2.3.6 Paracoccidioidomycosis (South American Blastomycosis) 42
2.3.7 Emmonsiosis 42
2.4 Opportunistic Fungal Infections 43
2.4.1 Aspergillosis (Alternaria) 43
2.4.2 Zygomycosis (Mucormycosis; Phycomycosis) 43
2.4.3 Hyalohyphomycoses. 44
2.4.4 Phaeohyphomycosis. 44
2.4.5 Protothecosis, Cutaneous 45
3 Viral Infections. 45
3.1 Herpes Viruses. 45
3.1.1 Herpes simplex (HSV-1, HSV-2). 45
3.1.2 Varizella/Zoster Virus Infection (VZV/HHV 3). 46
3.1.2.1 Varicella (Chickenpox). 46
3.1.2.2 Herpes Zoster (Shingles) 47
3.1.2.3 Special Feature: Necrotizing (Herpes) Zoster Folliculitis. 47
3.1.2.4 Special Feature: Zoster Associated Vasculitis 47
3.1.2.5 Postherpetic cutaneous reactions* 48
3.1.3 Burkitt Lymphoma; Epstein-Barr virus (HHV 4; Epstein-Barr Virus; EBV). 48
3.1.4 Hairy Leukoplakia (HHV 4; Epstein-Barr Virus; EBV). 49
3.1.5 Cytomegaly Virus (CMV; HHV 5) 49
3.1.6 Exanthema Subitum (HHV6) (Roseola Infantum, 6th Disease) 49
3.1.7 Pityriasis Rosea (HHV7) 50
3.1.8 AIDS-Kaposi Sarcoma (HHV8). 50
3.1.9 Multicentric Castleman’s Disease (HHV 8). 52
3.2 Human Papilloma Virus (HPV) Infections. 52
3.2.1 Verruca Vulgaris 53
3.2.2 Variant: Verrucae Planae 53
3.2.3 Variant: Condylomata acuminata 54
3.2.4 Differential Diagnosis: Acrokeratosis Verruciformis (Hopf) 54
3.2.5 Bowenoid Papulosis 54
3.2.6 Epidermodysplasia Verruciformis (Lewandowsky-Lutz); Verrucosis Generalisata. 54
3.3 Viral Exanthema. 55
3.3.1 Measles. 55
3.4 Parvovirus and Coxsackievirus Infections. 56
3.4.1 Erythema Infectiosum; (Slapped Cheek Disease; 5th Disease) 56
3.4.2 Papular Purpuric Gloves-and-Socks Syndrome 56
3.4.3 Hand-Foot-and-Mouth Disease (Coxsackie Virus) 56
3.5 Polyoma Virus Infections. 57
3.5.1-1 Trichodysplasia spinulosa 57
3.5.2 Merkel Cell Carcinoma (Primary Neuroendocrine Carcinoma of the Skin; Trabecular Carcinoma of Toker) 58
3.6 Poxviruses 59
3.6.1 Orthopox Virus Infections. 59
3.6.1.1 Cowpox (Catpox) 60
3.6.1.2 Vaccinia Inoculata 60
3.6.1.3 Smallpox (Variola Vera) 60
3.6.2 Parapox Virus Infections. 60
3.6.2.1 Ecthyma Contagiosum (Orf) 60
3.6.2.2 Variant: Milker’s Nodule. 61
3.6.2.3 Molluscum Contagiosum. 61
3.7 Other Skin Diseases with Suspected Viral Association 62
3.7.1 Asymmetric Periflexural Exanthema of Childhood 62
3.7.2 Eruptive Pseudoangiomatosis. 62
3.7.3 Gianotti-Crosti Syndrome. 63
3.7.4 Pityriasis Lichenoides (PL) 63
4 Parasitoses 64
4.1 Protozoan Diseases 64
4.1.1 Leishmaniasis. 64
4.1.2 Variant: Leishmania Mexicana. 65
4.1.3 Amebiasis: Entamoeba Histolytica. 66
4.1.4 Rhinosporidiosis. 66
4.2 Arthropod: Arachnids 66
4.2.1 Mites. 66
4.2.1.1 Demodex Folliculorum. 67
4.2.1.2 Scabies 67
4.2.1.3 Variant: Scabies Crustosa 68
4.2.1.4 Trombidiosis (Harvest mites; Chigger Itch) 68
4.2.2 Spiders* 68
4.2.3 Ticks*. 68
4.2.4 Insects. 69
4.2.5 Tungiasis (Sand Flea) 69
5 Helminthic Infections (Parasitic Worms). 69
5.1 Larva Migrans (Plumber’s Itch; Creeping Eruption). 70
5.2 Filariasis 70
5.3 Onchocerciasis (River Blindness) 70
5.4 Cysticercosis 71
5.5 Sparganosis 71
5.6 Schistosomiasis (Bilharziasis). 72
5.7 Cercarial Dermatitis (Swimmers Itch). 72
5.8 Annelida (ringed worms; segmented worms) *. 72
5.9 Hirudinea (Leeches) 73
6 Sepsis 73
6.1 Septic Vasculitis. 73
6.2. Bacterial Sepsis. 74
6.2.1 Gonococcal Sepsis 74
6.3 Fungal Sepsis. 74
6.3.1 Variant: Penicillium Marinum Sepsis. 74
6.3.2 Variant: Candida Sepsis 74
6.3.3 Variant: Aspergillus Sepsis 74
| Erscheinungsdatum | 09.03.2021 |
|---|---|
| Mitarbeit |
Chef-Herausgeber: Gunter Burg Mitglied der Redaktion: Heinz Kutzner, Werner Kempf, Josef Feit, Omar Sangueza |
| Verlagsort | Hoboken |
| Sprache | englisch |
| Maße | 179 x 260 mm |
| Gewicht | 618 g |
| Einbandart | gebunden |
| Themenwelt | Medizin / Pharmazie ► Allgemeines / Lexika |
| Medizin / Pharmazie ► Medizinische Fachgebiete ► Dermatologie | |
| Schlagworte | clinical microbiology • Dermatopathologie • Dermatopathology • Klinische Mikrobiologie • Medical Science • Medizin • Reise- u. Tropenmedizin • Travel / Tropical Medicine |
| ISBN-10 | 1-119-64706-1 / 1119647061 |
| ISBN-13 | 978-1-119-64706-5 / 9781119647065 |
| Zustand | Neuware |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
aus dem Bereich