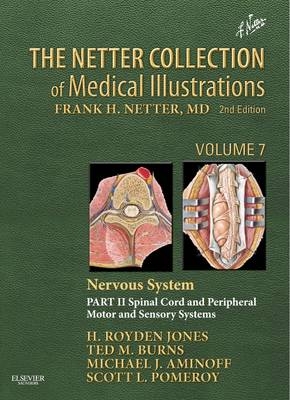
Netter Collection of Medical Illustrations: Nervous System
Saunders (Verlag)
978-1-4160-6386-5 (ISBN)
- Titel ist leider vergriffen;
keine Neuauflage - Artikel merken
"Spinal Cord and Peripheral Motor and Sensory Systems, Part 2" of "The Netter Collection of Medical Illustrations: Nervous System, 2nd Edition", provides a highly visual overview of the anatomy, pathology, and major clinical syndromes of the nervous system, from cranial nerves and neuro-ophthalmology to spinal cord, neuropathies, autonomic nervous system, pain physiology, and neuromuscular disorders. This spectacularly illustrated volume in the masterwork known as the (CIBA) Netter "Green Books" has been expanded and revised by Drs. H. Royden Jones, Jr., Ted M. Burns, Michael J. Aminoff, Scott L. Pomeroy to mirror the many exciting advances in neurologic medicine - offering rich insights into neuroanatomy, neurophysiology, molecular biology, pathology, and various clinical presentations.
Dr. Michael J. Aminoff is an internationally recognized, board-certified neurologist and clinical neurophysiologist who works at UCSF Medical Center and specializes in Parkinson's disease and other movement disorders, holding an endowed chair in Parkinson's disease research. Aminoff was educated in England, graduating with honors from University College in London in 1962 and as a physician from University College Hospital Medical School in 1965. He completed postdoctoral training in various London teaching hospitals, but especially at the National Hospital for Neurology and Neurosurgery in Queen Square, London, and at its affiliated Institute of Neurology, where his research on spinal physiology gained him an MD degree (an advanced research thesis in the UK). He joined UCSF Medical Center in 1974, becoming a full professor in 1982; the title of distinguished professor was conferred on him in 2010. In 2000, he was awarded a doctorate in science (an advanced doctorate in the Faculty of Science) from the University of London. He has received numerous awards including the Lifetime Achievement Award from the American Association of Neuromuscular & Electrodiagnostic Medicine (2006) and the A.B.Baker Award from the American Academy of Neurology (2007). He was the editor-in-chief of Muscle and Nerve, a major neuroscience journal for 10 years; serves on the editorial boards of several other medical and scientific journals; and has authored nearly 250 research publications as well as numerous books. Dr. Aminoff is also editor-in-chief of the Encyclopedia of Neurological Sciences and series editor of the multivolume Handbook of Clinical Neurology (Elsevier).
SECTION 1-CRANIAL NERVE AND NEURO-OPHTHALMOLOGIC DISORDERS OVERVIEW OF CRANIAL NERVES 1-1 Distribution of Motor and Sensory Fibers, 2 1-2 Nerves and Nuclei Viewed in Phantom from Behind, 4 1-3 Nerves and Nuclei in Lateral Dissection, 5 OLFACTORY (I) NERVE 1-4 Olfactory Pathways, 6 1-5 Olfactory Receptors, 7 1-6 Olfactory Bulb and Nerve, 8 OPTIC (II) NERVE 1-7 Eye, 9 1-8 Visual Pathways, 10 1-9 Optic Nerve Appearance, 11 1-10 Retinal Projections to Thalamus, Midbrain, and Brainstem, 12 1-11 Pupillary Light Reflex and the Accommodation Reflex, 13 OCULOMOTOR (III), TROCHLEAR (IV), AND ABDUCENS (VI) NERVES 1-12 Oculomotor (III), Trochlear (IV), and Abducens (VI) Nerves, 14 1-13 Nerves of Orbit and Cavernous Sinus, 15 1-14 Control of Eye Movements, 16 1-15 Control of Eye Movements-Pathology, 17 1-16 Control of Eye Movements-Pathology (Continued), 18 1-17 Autonomic Innervation of the Eye, 19 TRIGEMINAL (V) NERVE 1-18 Trigeminal (V) Nerve, 20 1-19 Trigeminal Nuclei: Afferent and Central Connections, 21 1-20 Trigeminal Nuclei: Central and Peripheral Connections, 22 1-21 Ophthalmic (V1) and Maxillary (V2) Nerves, 23 1-22 Mandibular Nerve (V3), 24 1-23 Trigeminal Nerve Disorders, 25 FACIAL (VII) NERVE 1-24 Facial (VII) Nerve, 26 1-25 Muscles of Facial Expression: Lateral View, 27 1-26 Central Versus Peripheral Facial Paralysis, 28 1-27 Facial Palsy, 29 TASTE RECEPTORS AND PATHWAYS 1-28 Anatomy of Taste Buds and Their Receptors, 30 1-29 Tongue, 31 VESTIBULOCOCHLEAR (VIII) NERVE 1-30 Vestibulocochlear (VIII) Nerve, 32 1-31 Pathway of Sound Reception, 33 1-32 Pathologic Causes of Vertigo, 34 1-33 Canalith Repositioning (Epley Maneuver), 35 1-34 Afferent Auditory Pathways, 36 1-35 Centrifugal Auditory Pathways, 37 1-36 Vestibular Receptors, 38 1-37 Cochlear Receptors, 39 GLOSSOPHARYNGEAL (IX) NERVE 1-38 Glossopharyngeal (IX) Nerve, 40 1-39 Otic Ganglion, 41 VAGUS (X) NERVE 1-40 Vagus (X) Nerve, 42 1-41 Vagus Nerve Branches and Disorders, 43 ACCESSORY (XI) NERVE 1-42 Accessory (XI) Nerve, 44 1-43 Clinical Findings in Cranial Nerve XI Damage, 45 HYPOGLOSSAL (XII) NERVE 1-44 Hypoglossal (XII) Nerve, 46 1-45 Intramedullary Course, 47 1-46 Disorders of Hypoglossal Nucleus and Nerve, 48 SECTION 2-SPINAL CORD: ANATOMY AND MYELOPATHIES 2-1 Spinal Cord, 50 2-2 Spinal Membranes and Nerve Roots, 51 2-3 Arteries of Spinal Cord, 52 2-4 Arteries of Spinal Cord: Intrinsic Distribution, 53 2-5 Veins of Spinal Cord, Nerve Roots, and Vertebrae, 54 2-6 Principal Fiber Tracts of Spinal Cord, 55 2-7 Somesthetic System of Body, 56 2-8 Corticospinal (Pyramidal) System: Motor Component, 57 2-9 Rubrospinal Tract, 58 2-10 Vestibulospinal Tracts, 59 2-11 Reticulospinal and Corticoreticular Pathways, 60 2-12 Spinal Origin or Termination of Major Descending Tracts and Ascending Pathways, 61 2-13 Cytoarchitecture of Spinal Cord Gray Matter, 62 2-14 Spinal Effector Mechanisms, 63 2-15 Spinal Reflex Pathways, 64 2-16 Motor Impairment Related to Level of Spinal Cord Injury, 65 2-17 Sensory Impairment Related to Level of Spinal Cord Injury, 66 2-18 Incomplete Spinal Cord Syndromes, 67 2-19 Acute Spinal Cord Syndromes: Evolution of Symptoms, 68 2-20 Acute Spinal Cord Syndromes: Pathology, Etiology, and Diagnosis, 69 2-21 Spinal Tumors, 70 2-22 Spinal Tumors (Continued), 71 2-23 Neuroimaging (MRI) Characteristics of Spinal Tumors, 72 2-24 Syringomyelia, 73 2-25 Subacute Combined Degeneration, 74 2-26 Spinal Dural Fistulas and Arteriovenous Malformations, 75 2-27 Cervical Spondylosis, 76 2-28 Cervical Disk Herniation Causing Cord Compression, 77 2-29 Infectious and Hereditary Myelopathies, 78 SECTION 3-SPINAL TRAUMA 3-1 Spinal Column, 80 3-2 Atlas and Axis, 81 3-3 Cervical Vertebrae, 82 3-4 External Craniocervical Ligaments, 83 3-5 Internal Craniocervical Ligaments, 84 3-6 Thoracic Vertebrae, 85 3-7 Lumbar Vertebrae and Intervertebral Disk, 86 3-8 Ligaments of Spinal Column, 87 3-9 Sacrum and Coccyx, 88 3-10 Ligaments of Sacrum and Coccyx, 89 3-11 Distractive Flexion, 90 3-12 Compressive Flexion, 91 3-13 Distractive Extension, 92 3-14 Cervical Spine Injury: Prehospital, Emergency Room, and Acute Management, 93 3-15 Traction and Bracing, 94 3-16 Anterior Cervical Spine Decompression and Stabilization, 95 3-17 Posterior Cervical Stabilization and Fusion, 96 3-18 Spinal Cord Injury Medical Issues, 97 SECTION 4-NERVE ROOTS AND PLEXUS DISORDERS 4-1 Cervical Disk Herniation, 100 4-2 Radiographic Diagnosis of Radiculopathy, 101 4-3 Examination of Patient with Low Back Pain, 102 4-4 Lumbar Disk Herniation: Clinical Manifestations, 103 4-5 L4-5 Disk Extrusion, 104 4-6 Lumbosacral Spinal Stenosis, 105 4-7 Spinal Nerves, 106 4-8 Dermal Segmentation, 107 4-9 Thoracic Nerves, 108 4-10 Thoracic Spinal Nerve Root Disorders, 109 4-11 Diabetic Lumbosacral Radiculoplexus Neuropathy, 110 4-12 Lumbar, Sacral, and Coccygeal Plexuses, 111 4-13 Brachial Plexus, 112 4-14 Brachial Plexus and/or Cervical Nerve Root Injuries at Birth, 113 4-15 Brachial Plexopathy, 114 4-16 Lumbosacral Plexopathy, 115 4-17 Cervical Plexus, 116 SECTION 5-MONONEUROPATHIES 5-1 Compression Neuropathies, 118 5-2 Chronic Nerve Compression, 119 5-3 Electrodiagnostic Studies in Compression Neuropathy, 120 5-4 Radiologic Studies in Compression Neuropathy, 121 5-5 Proximal Nerves of the Upper Extremity: Spinal Accessory Nerve, 122 5-6 Proximal Nerves of the Upper Extremity: Suprascapular and Musculocutaneous Nerves, 123 5-7 Median Nerve, 124 5-8 Proximal Median Neuropathies, 125 5-9 Distal Median Nerve, 126 5-10 Distal Median Neuropathies: Carpal Tunnel Syndrome, 127 5-11 Proximal Ulnar Nerve, 128 5-12 Ulnar Mononeuropathies: Potential Entrapment Sites, 129 5-13 Radial Nerve, 130 5-14 Radial Nerve Compression/Entrapment Neuropathies, 131 5-15 Femoral and Lateral Femoral Cutaneous Nerves, 132 5-16 Iliohypogastric, Ilioinguinal, Genitofemoral, and Obturator Nerves, 133 5-17 Gluteal Nerves, 134 5-18 Sciatic and Posterior Femoral Cutaneous Nerves, 135 5-19 Fibular (Peroneal) Nerve, 136 5-20 Tibial Nerve, 137 5-21 Cutaneous Innervation, 138 5-22 Dermatomes, 139 SECTION 6-PERIPHERAL NEUROPATHIES 6-1 Anatomy of Peripheral Nerve, 143 6-2 Histology of Peripheral Nerve, 144 6-3 Cell Types of Nervous System, 145 6-4 Resting Membrane Potential, 146 6-5 Ion Channel Mechanics and Action Potential Generation, 147 6-6 Neurophysiology and Peripheral Nerve Demyelination, 148 6-7 Impulse Propagation, 149 6-8 Conduction Velocity, 150 6-9 Visceral Efferent Endings, 151 6-10 Cutaneous Receptors, 152 6-11 Pacinian Corpuscle, 153 6-12 Muscle and Joint Receptors, 154 6-13 Proprioceptive Reflex Control of Muscle Tension, 155 6-14 Hereditary Motor and Sensory Neuropathies (HMSN, i.e., Charcot-Marie- Tooth Disease), 156 6-15 Hereditary Motor and Sensory Neuropathy Types I and II, 157 6-16 Other Hereditary Motor and Sensory Neuropathies (Types III, IV, and X), 158 6-17 Hereditary Sensory and Autonomic Neuropathy, 159 6-18 Guillain-Barre Syndrome, 160 6-19 Guillain-Barre Syndrome (Continued), 161 6-20 Chronic Inflammatory Demyelinating Polyradiculoneuropathy, 162 6-21 Diabetic Neuropathies, 163 6-22 Monoclonal Protein-Associated Neuropathies: Amyloid Neuropathy, 164 6-23 Monoclonal Protein-Associated Neuropathies: Distal Acquired Demyelinating Symmetric (DADS) Neuropathy, 165 6-24 Vasculitic Neuropathy and Other Connective Tissue Disorders Associated with Neuropathy: Fibrinoid Necrosis, 166 6-25 Vasculitic Neuropathy and Other Connective Tissue Disorders Associated with Neuropathy: Sjogren Syndrome, 167 6-26 Immunopathogenesis of Guillain-Barre Syndrome, 168 6-27 Peripheral Neuropathy Cause by Heavy Metal Poisoning, 169 6-28 Metabolic, Toxic, and Nutritional Peripheral Neuropathies, 170 6-29 Leprosy and Other Infections Sometimes Causing Peripheral Neuropathies, 171 SECTION 7-AUTONOMIC NERVOUS SYSTEM AND ITS DISORDERS 7-1 General Topography of Autonomic Nervous System, 174 7-2 General Topography of Autonomic Nervous System (Continued), 175 7-3 Autonomic Reflex Pathways, 176 7-4 Cholinergic and Adrenergic Nerves, 177 7-5 Autonomic Nerves in Head, 178 7-6 Autonomic Nerves in Neck, 179 7-7 Autonomic Distribution to the Head and the Neck, 180 7-8 Ciliary Ganglion, 181 7-9 Thoracic Sympathetic Chain and Splanchnic Nerves, 182 7-10 Innervation of Heart, 183 7-11 Innervation of Blood Vessels, 184 7-12 Carotid Body and Carotid Sinus, 185 7-13 Autonomic Nerves and Ganglia in Abdomen, 186 7-14 Innervation of Stomach and Proximal Duodenum, 187 7-15 Innervation of Intestines, 188 7-16 Autonomic Innervation of Small Intestine, 189 7-17 Enteric Plexuses, 190 7-18 Innervation of Liver and Biliary Tract, 191 7-19 Innervation of Adrenal Glands, 192 7-20 Autonomic Nerves and Ganglia in Pelvis, 193 7-21 Autonomic Innervation of Kidneys and Upper Ureters, 194 7-22 Innervation of Urinary Bladder and Lower Ureter, 195 7-23 Innervation of Male Reproductive Organs, 196 7-24 Innervation of Female Reproductive Organs, 197 7-25 Autonomic Testing, 198 7-26 Abnormal Pupillary Conditions, 199 7-27 Clinical Presentation of Autonomic Disorders, 200 SECTION 8-PAIN 8-1 Somatosensory System, 202 8-2 Somatosensory Afferents and Principal Fiber Tracts, 203 8-3 Pain Pathways, 204 8-4 Endorphin System, 205 8-5 Spinothalamic and Spinoreticular Nociceptive Processing in the Spinal Cord, 206 8-6 Central Nervous System Neurotransmitters, Receptors, and Drug Targets, 207 8-7 Thalamic Pain Syndrome, 208 8-8 Clinical Manifestations Related to Thalamus Site in Intracerebral Hemorrhage, 209 8-9 Complex Regional Pain, 210 8-10 Herpes Zoster, 211 8-11 Occipital Neuralgia, 212 8-12 Myofascial Factors in Low Back Pain, 213 8-13 Myofascial Factors in Low Back Pain (Continued): Posterior Abdominal Wall: Internal View, 214 8-14 Lumbar Zygapophyseal Joint Back Pain, 215 8-15 Low Back Pain and Effects of Lumbar Hyperlordosis and Flexion on Spinal Nerves, 216 8-16 Examination of the Low Back Pain Patient, 217 8-17 Osteoporosis, 218 8-18 Diagnosis of Hip, Buttock, and Back Pain, 219 8-19 Hip Joint Involvement in Osteoarthritis, 220 8-20 Peripheral Nerves of Feet, Painful Peripheral Neuropathies, 221 8-21 Peripheral Neuropathies: Clinical Manifestations, 222 8-22 Neurologic Evaluation of the Somatoform Patient: Cutaneous Distribution of Peripheral Nerves, 223 8-23 Neurologic Evaluation of the Somatoform Patient: Somatoform Conversion Reactions, 224 SECTION 9-FLOPPY INFANT 9-1 Neonatal Hypotonia, 226 9-2 Spinal Muscular Atrophy Type I (Werdnig- Hoffmann Disease), 227 9-3 Infantile Neuromuscular Junction (NMJ) Disorders, 228 9-4 Congenital Myopathies, 229 9-5 Arthrogryposis Multiplex Congenita, 230 SECTION 10-MOTOR NEURON AND ITS DISORDERS 10-1 Peripheral Nervous System: Overview, 232 10-2 Spinal Cord and Neuronal Cell Body with Motor, Sensory, and Autonomic Components of the Peripheral Nerve, 233 10-3 Motor Unit, 234 10-4 Motor Unit Potentials, 235 10-5 Primary Motor Neuron Disease, 236 10-6 Clinical Manifestations of Amyotrophic Lateral Sclerosis, 237 10-7 Clinical Manifestations of Amyotrophic Lateral Sclerosis (Continued), 238 10-8 Mimics of Amyotrophic Lateral Sclerosis, 239 10-9 Diagnosis of Amyotrophic Lateral Sclerosis, 240 10-10 Treatment of Amyotrophic Lateral Sclerosis, 241 10-11 Spinal Muscular Atrophy and Spinal Bulbar Muscular Atrophy, 242 SECTION 11-NEUROMUSCULAR JUNCTION AND ITS DISORDERS 11-1 Structure of Neuromuscular Junction, 244 11-2 Physiology of Neuromuscular Junction, 245 11-3 Somatic Neuromuscular Transmission, 246 11-4 Pharmacology of Neuromuscular Transmission, 247 11-5 Repetitive Motor Nerve Stimulation, 248 11-6 Myasthenia Gravis: Clinical Manifestations, 249 11-7 Myasthenia Gravis: Etiologic and Pathophysiologic Concepts, 250 11-8 Immunopathology of Myasthenia Gravis, 251 11-9 Presynaptic Neuromuscular Junction Transmission Disorders: Lambert-Eaton Myasthenic Syndrome and Infantile Botulism, 252 11-10 Congenital Myasthenic Syndromes, 253 11-11 Foodborne Neurotoxins, 254 SECTION 12-MUSCLE AND ITS DISORDERS 12-1 Muscle Fiber Anatomy: Basic Sarcomere Subdivisions, 256 12-2 Muscle Fiber Anatomy: Biochemical Mechanics of Contraction, 257 12-3 Muscle Membrane, T Tubules, and Sarcoplasmic Reticulum, 258 12-4 Muscle Response to Nerve Stimulation, 259 12-5 Metabolism of Muscle Cell, 260 12-6 Muscle Fiber Types, 261 12-7 Overview of Myopathies: Clinical Approach, 262 12-8 Dystrophinopathies: Duchenne Muscular Dystrophy-Gower's Maneuver, 264 12-9 Dystrophinopathies: Duchenne Muscular Dystrophy, 265 12-10 Dystrophinopathies: Molecular Genetic Testing, 266 12-11 Myotonic Dystrophy and Other Myotonic Disorders, 267 12-12 Myotonic Dystrophy and Other Myotonic Disorders (Continued), 268 12-13 Other Types of Muscular Dystrophy, 269 12-14 Polymyositis and Dermatomyositis, 270 12-15 Polymyositis and Dermatomyositis (Continued), 271 12-16 Inclusion Body Myositis, 272 12-17 Immunopathology for Inflammatory Myopathies, 273 12-18 Endocrine, Toxic, and Critical Illness Myopathies, 274 12-19 Myopathies: Hypokalemia/Hyperkalemia and the Periodic Paralyses Channelopathies Myopathies Associated with Disorders of Potassium Metabolism, 275 12-20 Metabolic and Mitochondrial Myopathies, 276 12-21 Myoglobinuric Syndromes Including Malignant Hyperthermia, 277
| Erscheint lt. Verlag | 11.3.2013 |
|---|---|
| Reihe/Serie | Netter Green Book Collection |
| Zusatzinfo | Approx. 300 illustrations (300 in full color) |
| Verlagsort | Philadelphia |
| Sprache | englisch |
| Maße | 247 x 299 mm |
| Gewicht | 1488 g |
| Themenwelt | Medizin / Pharmazie ► Medizinische Fachgebiete ► Neurologie |
| Studium ► 1. Studienabschnitt (Vorklinik) ► Anatomie / Neuroanatomie | |
| ISBN-10 | 1-4160-6386-2 / 1416063862 |
| ISBN-13 | 978-1-4160-6386-5 / 9781416063865 |
| Zustand | Neuware |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
aus dem Bereich