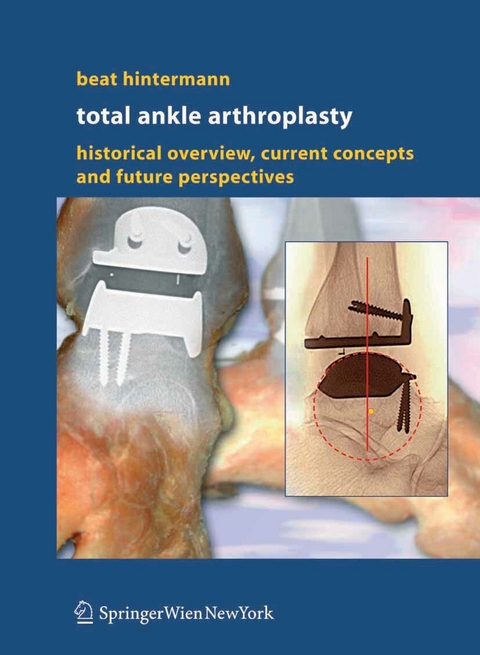
Total Ankle Arthroplasty (eBook)
XVIII, 195 Seiten
Springer Wien (Verlag)
978-3-211-27254-1 (ISBN)
Foreword 7
Acknowledgements 9
Preface 11
Contents 13
Chapter 1 Introduction 19
1.1 Why Total Ankle Arthroplasty? 19
1.2 Poor Success Rate with Early Attempts 20
1.3 Where Are We Today? 20
References 21
Chapter 2 Characteristics of the Diseased Ankle 23
2.1 Epidemiology 23
2.2 Characteristics of Ankle Arthritis 23
2.2.1 Primary Osteoarthrosis 26
2.2.2 Post-Traumatic Osteoarthrosis 26
2.2.3 Systemic Arthritis 27
2.3 Conclusions 27
References 27
Chapter 3 Ankle Arthrodesis 29
3.1 Historical Background 29
3.2 Biomechanical Considerations 30
3.2.1 Isolated Ankle Arthrodesis 31
3.2.2 Extensive Hindfoot Fusions 31
3.3 Techniques and Results 31
3.3.1 Ankle Arthrodesis without Internal Fixation 32
3.3.2 Ankle Arthrodesis with Internal Fixation 32
3.3.3 Functional Outcome after Ankle Arthrodesis 35
3.3.4 Degenerative Changes after Ankle Arthrodesis 36
3.3.5 Ankle Arthrodesis versus Total Ankle Arthroplasty 37
3.4 Conclusions 39
References 39
Chapter 4 Anatomic and Biomechanical Characteristics of the Ankle Joint and Total Ankle Arthroplasty 43
4.1 Anatomic Considerations 43
4.1.1 Bony Configuration 43
4.1.2 Ligamentous Configuration 45
4.2 Ankle Joint Motion 47
4.2.1 Axis of Rotation 47
4.2.2 Range of Ankle Motion 48
4.2.3 Restraints of Ankle Motion 48
4.3 Bone Support at the Ankle 49
4.4 Contact Area and Forces at the Ankle 52
4.4.1 Contact Area 52
4.4.2 Axial Load and Stress Forces of the Ankle 52
4.5 Fixation of Total Ankle Prostheses 53
4.6 Limitations of Polyethylene 55
4.7 Component Design 55
4.8 Conclusions 57
References 58
Chapter 5 History of Total Ankle Arthroplasty 61
5.1 Classification of Total Ankle Arthroplasties 61
5.2 First-Generation Total Ankle Arthroplasty – Cemented Type 63
5.2.1 Pioneers in Total Ankle Arthroplasty 63
5.2.2 Short-Term Results 65
5.2.3 Mid- to Long-Term Results 65
5.2.4 Specific Problems with Early Use of Total Ankle Implants 66
5.3 Second-Generation Total Ankle Arthroplasty – Uncemented Type 67
5.3.1 Basic Biomechanical Considerations in New Prosthetic Designs 67
5.3.2 Two-Component Designs 68
5.3.3 Three-Component Designs 69
5.3.4 First Results 69
5.3.5 Critical Issues in Second-Generation Total Ankle Replacement 70
5.4 Conclusions 71
References 71
Chapter 6 Current Designs of Total Ankle Prostheses 77
6.1 AES® Ankle 77
6.1.1 Background and Design 77
6.1.2 Results 78
6.1.3 Concerns 78
6.2 AGILITY Ankle 79
6.2.1 Background and Design 79
6.2.2 Results 80
6.2.3 Concerns 81
6.3 Buechel-Pappas Ankle 82
6.3.1 Background and Design 82
6.3.2 Results 83
6.3.3 Concerns 84
6.4 ESKA Ankle 86
6.4.1 Background and Design 86
6.4.2 Results 86
6.4.3 Concerns 88
6.5 HINTEGRA® Ankle 88
6.5.1 Background and Design 88
6.5.2 Results 90
6.5.3 Concerns 90
6.6 Ramses Ankle 93
6.6.1 Background and Design 93
6.6.2 Results 95
6.6.3 Concerns 95
6.7 SALTO® Ankle 96
6.7.1 Background and Design 96
6.7.2 Results 96
6.7.3 Concerns 96
6.8 S.T.A.R. Ankle 98
6.8.1 Background and Design 98
6.8.2 Results 99
6.8.3 Concerns 100
6.9 TNK Ankle 102
6.9.1 Background and Design 102
6.9.2 Results 102
6.9.3 Concerns 105
6.10 Conclusions 105
References 106
Chapter 7 Preoperative Considerations for Total Ankle Arthroplasty 109
7.1 Indications 109
7.2 Contraindications 110
7.3 Considerations Specific to Total Ankle Replacement Surgery 111
7.3.1 Rheumatoid Arthritis and Inflammatory Arthropathy 111
7.3.2 Infection 111
7.3.3 Osteopenia and Osteoporosis 113
7.3.4 Weight Restrictions 113
7.3.5 Adjacent Joint Arthritis 115
7.3.6 Lower Limb, Ankle, or Hindfoot Malalignment 116
7.3.7 Hindfoot-Ankle Instability 116
7.3.8 Heel Cord Contracture 119
7.3.9 Soft-Tissue Considerations 119
7.3.10 Age Considerations 119
7.3.11 Activity Limitations 120
7.3.12 Smoking 121
7.4 Conclusions 121
References 121
Chapter 8 Surgical Techniques 123
8.1 Preoperative Planning 123
8.2 Surgical Approach to the Ankle 123
8.2.1 Anterior Approach to the Ankle 123
8.2.2 Lateral Approach to the Ankle 126
8.2.3 Complications 126
8.3 Surgical Preparation of the Ankle 126
8.4 Insertion of the Implants 131
8.5 Wound Closure 134
8.6 Additional Surgeries 135
8.6.1 Lateral Ligament Reconstruction 135
8.6.2 Peroneal Tendon Transfer 137
8.6.3 Dorsiflexion Osteotomy of the First Metatarsal 137
8.6.4 Valgisation Osteotomy of the Calcaneus 138
8.6.5 Medial Ligament Reconstruction 138
8.6.6 Medial Sliding Osteotomy of the Calcaneus 138
8.6.7 Hindfoot Fusion 138
8.6.8 Heel Cord Lengthening 139
8.7 Conclusions 139
References 144
Chapter 9 Postoperative Care and Follow-up 145
9.1 Postoperative Care 145
9.2 Rehabilitation Program 146
9.3 Follow-up Examination 146
9.3.1 Clinical Assessment 146
9.3.2 Radiographic Measurements 147
9.4 Conclusions 151
References 151
Chapter 10 What is Feasible in Total Ankle Arthroplasty? 153
10.1 Reconstruction of the Malaligned Ankle 153
10.1.1 Varus Malalignment 153
10.1.2 Valgus Malalignment 157
10.1.3 Sagittal Plane Malalignment 159
10.2 Reconstruction of the Post-Traumatic Hindfoot and Ankle 159
10.2.1 Fibular Malunion 160
10.2.2 Tibiofibular Instability (Syndesmotic Incompetence) 162
10.2.3 Calcaneal Malunion 163
10.3 Specific Articular Pathologies and Disorders 168
10.3.1 Systemic Inflammatory Arthritis 168
10.3.2 Clubfoot Deformity 170
10.3.3 Post-Polio Foot Deformity 170
10.3.4 Avascular Necrosis 170
10.3.5 Septic Arthritis 173
10.4 Disarthrodesis 176
10.5 Revision Arthroplasty (for Failed Primary Arthroplasty) 177
10.6 Conclusions 180
Chapter 11 Complications of Total Ankle Arthroplasty 181
11.1 Characteristics of Ankle Osteoarthritis 181
11.1.1 Primary Osteoarthrosis of the Ankle 181
11.1.2 Post-Traumatic Osteoarthrosis of the Ankle 181
11.1.3 Rheumatoid Arthritis of the Ankle 181
11.2 Patient Selection 183
11.2.1 Age of the Patient 183
11.2.2 Weight of the Patient 183
11.3 Preoperative Conditions and Planning 183
11.3.1 Soft-Tissue Conditions 183
11.3.2 Malalignment and Malunion 183
11.3.3 Preoperative Foot Deformity 185
11.4 Implant- and Implantation-Related Complications 186
11.4.1 Problems with First-Generation Total Ankle Prostheses 186
11.4.2 Problems with Second-Generation Total Ankle Prostheses 186
11.5 Early Postoperative Complications 193
11.5.1 Wound Healing Problems 193
11.5.2 Swelling 194
11.5.3 Infection 194
11.5.4 Deep Venous Thrombosis 194
11.5.5 Syndesmotic Nonunion / Instability 194
11.5.6 Fractures of Malleoli 194
11.6 Late Postoperative Complications 194
11.6.1 Loss of Motion 194
11.6.2 Aseptic Loosening 196
11.6.3 Subsidence 198
11.6.4 Polyethylene Wear 199
11.7 Salvage of Failed Total Ankle Arthroplasty 199
11.8 Conclusions 199
11.8.1 Requirements for Successful Total Ankle Arthroplasty 201
11.8.2 Surgeon Experience, Skill, and Training 201
References 201
Chapter 12 Future Directions 203
12.1 Current Concerns to be Addressed 203
12.1.1 Prospective Studies 203
12.1.2 Prosthetic Design 203
12.1.3 Preoperative Planning and Implantation Technique 203
12.1.4 Polyethylene Wear 204
12.1.5 Stability of Bone-Implant Interface 204
12.2 Further Success will Increase Patient Demand 204
12.3 Further Research 204
12.4 Conclusions 205
Subject Index 207
Chapter 8 SURGICAL TECHNIQUES (p. 105)
Although many surgical approaches have been described in the literature, most current total ankle prostheses are implanted using the standard anterior ankle approach. Because of the fragility of the soft tissues around the ankle, however, and scars from previous injuries or surgeries, the approach sometimes demands a modified technique in order to prevent wound healing problems. Various techniques are used to implant current ankle prostheses. In most cases, however, a jig is used to align a tibial resection block with respect to the longitudinal axis of the tibia. Talar resection is made, to some extent, as a free-hand surgery. In some cases (with the AGILITYTM ankle, for example), an external fixator/ distractor is used to realign the ankle and tension the ligaments.
8.1 Preoperative Planning
Recognizing critical preoperative risk factors and doing careful preoperative planning are important factors for limiting complications and obtaining satisfactory results. Meticulous clinical and radiological assessment is required. Clinically, the surgeon should examine and document the softtissue conditions, hindfoot alignment, ankle stability, foot deformities, foot vascularization, and sensibility. Lateral and anteroposterior weightbearing radiographs of the foot and ankle are mandatory, and may help to identify possible osteoarthritis in adjacent joints, as well as varus and valgus deformities of the hindfoot and longitudinal arch. The use of MRI may also help to determine the condition of the subchondral bone, particularly with respect to potential osteonecrosis.
8.2 Surgical Approach to the Ankle
Most of the current total ankle prostheses (the Buechel-PappasTM ankle [15], the HINTEGRA® ankle [8], the TNK ankle [19], the Ramses ankle [16], the SALTO® ankle [2], and the S.T.A.R. ankle [14]) are implanted using the standard anterior ankle approach, which uses a single incision between the anterior tibial and extensor hallucis longus tendons. The AGILITYTM ankle uses the same anterior incision, as well as a lateral incision over the distal fibula to mobilize and bridge the tibiofibular syndesmosis [17]. The ESKA ankle, by contrast, is implanted using a single lateral (transfibular) approach [18].
8.2.1 Anterior Approach to the Ankle
The patient is positioned supine, with the heel of the foot on the edge of the table. A support beneath the ipsilateral hip, and/or tilting the table serves to get the foot in an upright position so that the ankle is seen from the front side of the leg (Fig. 8.1). A longitudinal skin incision is made over the center of the ankle (Fig. 8.2), taking care to identify and retract the medial branch of the superficial peroneal nerve (Fig. 8.3). The approach is made longitudinally between the extensor hallucis longus and anterior tibial tendons, through the tendon sheet of the extensor hallucis longus [5, 21] or of the anterior tibial tendon [8, 10]. Once the distal tibia is exposed just beneath the anterior tibial tendon ("safety area"), the soft tissues are pushed sideways using a raspatory subperiosteally. Then, the neurovascular bundle is retracted laterally, and two Hohmann retractors are inserted (Fig. 8.4). The ankle capsule is incised vertically over the midpoint of the ankle. Note that it may be necessary to excise the central part of this capsule to gain good exposure.
| Erscheint lt. Verlag | 16.6.2005 |
|---|---|
| Zusatzinfo | XVIII, 195 p. With zahlreichen z.T. farb. Abb. |
| Verlagsort | Vienna |
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Medizinische Fachgebiete ► Chirurgie |
| Medizin / Pharmazie ► Medizinische Fachgebiete ► Orthopädie | |
| Schlagworte | ankle • ankle arthrodesis • ankle joint • Arthroplasty • Biomechanics • implants • joints |
| ISBN-10 | 3-211-27254-2 / 3211272542 |
| ISBN-13 | 978-3-211-27254-1 / 9783211272541 |
| Informationen gemäß Produktsicherheitsverordnung (GPSR) | |
| Haben Sie eine Frage zum Produkt? |
Größe: 7,2 MB
DRM: Digitales Wasserzeichen
Dieses eBook enthält ein digitales Wasserzeichen und ist damit für Sie personalisiert. Bei einer missbräuchlichen Weitergabe des eBooks an Dritte ist eine Rückverfolgung an die Quelle möglich.
Dateiformat: PDF (Portable Document Format)
Mit einem festen Seitenlayout eignet sich die PDF besonders für Fachbücher mit Spalten, Tabellen und Abbildungen. Eine PDF kann auf fast allen Geräten angezeigt werden, ist aber für kleine Displays (Smartphone, eReader) nur eingeschränkt geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen dafür einen PDF-Viewer - z.B. den Adobe Reader oder Adobe Digital Editions.
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen dafür einen PDF-Viewer - z.B. die kostenlose Adobe Digital Editions-App.
Zusätzliches Feature: Online Lesen
Dieses eBook können Sie zusätzlich zum Download auch online im Webbrowser lesen.
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich