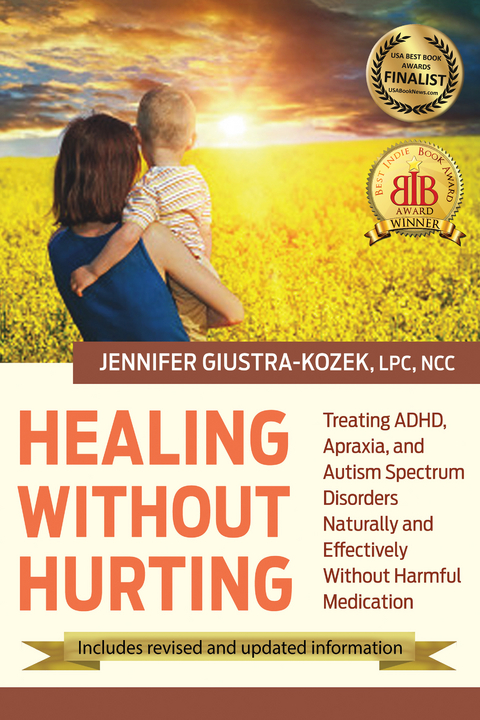
2 pack Ultimate Fashion books (eBook)
384 Seiten
Changing Lives Press (Verlag)
978-0-9904396-1-5 (ISBN)
Jennifer Giustra-Kozek is a therapist who practices in Connecticut, and is also the mother of a son with Autism Spectrum disorders. After treating Evan bio-medically, along with other healing practices, Jennifer witnessed the kind of improvements that every parent of a similarly diagnosed child dreams of: Evan no longer grunts and screams, throws toys, hits others, or has mood swings. He no longer throws himself into fits of uncontrollable rage, listens to his teachers & responds appropriately. He copes better with changes in routine & makes eye contact more often. He no longer enters into a trance-like state ...and the list goes on. Healing without Hurting includes a full menu of natural treatment options, including: A real world success story and simple recipes/healthy alternatives. Readers will learn how to: Identify common labels of behaviorsRecognize the early warning signs that an autoimmune disorder is brewing Identify the different medications; potential benefits and side-effects Find the right doctors and practitioners Identify food sensitivities and other autoimmune assaults and much more.....
CHAPTER 1
Our Journey Begins
At thirty-two weeks pregnant, I found myself up in bed at 4:00 a.m. counting my contractions. Could I be going into labor eight weeks prematurely? By coincidence, my next gynecologist appointment was for that morning at 10:00 a.m. When I told the doctor my suspicions, she replied, “Oh, no, you’re much too early. These must be Braxton Hicks contractions.” But my body and instincts told me differently.
After twenty minutes in her office, my doctor wanted to send me home without completing an internal exam. I refused to leave. It was the first of a number of decisions contrary to doctor’s orders that would save Evan’s life.
After completing an internal exam, my doctor confirmed that I really was in labor. She told me to go across the street to the hospital. While the contractions intensified, I drove my car to the hospital’s parking garage. As I waited by the hospital elevator, I pulled out my cell phone to reach my husband, Steve. Then I noticed a sign saying the elevator was out of order. In a panic, I began walking five long flights of stairs to the maternity floor.
I could feel that something wasn’t right. The nurses hooked me up to a monitor and gave me an ultrasound immediately. It was bad news—little Evan was positioned with his butt down and his legs over his head like a jackknife. Luckily, the nurses told me his heartbeat was going strong, and they’d try to stop the contractions.
Steve arrived but couldn’t do much other than comfort me. Still, that counted for a lot.
At 8:00 p.m., Steve left to get a bite to eat at a local Mexican restaurant. I hadn’t eaten anything all morning, and since I might end up needing surgery, no one would feed me. I was starving.
As I waited for Steve, a doctor came in and told me they needed to keep me overnight because the contractions weren’t slowing down as quickly as they had hoped. I began to worry that my instincts were right. I remembered how many times I had gone for fetal movement tests, concerned something was wrong with my son. I had never felt butterflies fluttering or those reassuring kicks everyone always talked about.
Steve returned within an hour and helped me get to the bathroom, despite the fact that I was hooked up to a bunch of IVs and monitor leads. When I returned to bed, I heard alarms, and hospital personnel scrambled into my room. I felt like my body was no longer my own. An oxygen mask was strapped around my mouth and nose. As tears ran down my face, I saw Steve being escorted out. An anesthesiologist asked me to roll onto my side, and he jammed an epidural into my spine. Within minutes, I couldn’t feel my legs, and the doctors were performing an emergency Caesarean section.
My tiny baby boy was delivered within minutes, weighing four pounds, two ounces. I had one quick look at him before he was taken away by the neonatal intensive care unit (NICU) team. He had a full head of dark hair and a slightly flattened little nose.
I was told later that the team had needed to act quickly because his umbilical cord had been wrapped so tightly around his little body that it had caused his oxygen levels to drop. The medical team needed to work on him for quite a while.
How did this happen?
I was thirty-two when Steve and I tried to start a family. I considered myself relatively healthy. I had been on birth control pills for fifteen years and expected that, after being on them for so long, pregnancy would happen rather quickly. It actually took eight months to get the good news. I scheduled a GYN appointment to discuss infertility treatment options, and it was during that appointment that the nurse informed me I was approximately six weeks pregnant. A blood test confirmed the findings. Steve and I were elated.
I ate relatively well and exercised regularly during my pregnancy. I took my natural, whole-food prenatal vitamins after hearing that they were more bioavailable and contained more B “brain” vitamins than many of the prescribed counterparts. I also took omega-3 fish oil for over a year, and I followed all of the prenatal guidelines. I attended every scheduled appointment, drank plenty of water, and avoided raw eggs, tuna, and other big fish that could contain mercury. I avoided over-the-counter medications and alcohol, and I refused to get my hair dyed.
I had terrible heartburn, however, so my doctor insisted that taking an antacid was absolutely acceptable. I popped them like candy on some days without realizing how much aluminum they contain. (It wasn’t until recently that I learned that too much aluminum can affect a baby’s developing brain. Nor did I know that antacids, especially ones that contain aluminum, can interfere with iron, calcium, zinc, and magnesium absorption and function.) I had little nausea throughout my pregnancy, but perhaps some afternoon queasiness if I hadn’t eaten. My blood pressure was always on the low to normal side.
With every ultrasound, I was reassured that my little baby was growing normally. I was at the doctor’s office often so that they could perform a stress test or an additional ultrasound to monitor fetal movement. Each time, they told me that the baby’s heartbeat was strong and that everything was all right. At twenty weeks, it was confirmed that I was having a little boy, and I started preparing his nursery. Most of my pregnancy was uneventful until the unforeseen happened.
Neonatal Intensive Care Unit (NICU)
Evan spent five and a half weeks in the NICU, mostly in an incubator. As a premature baby, his lungs were underdeveloped, and he lacked coordination for sucking, swallowing, and breathing. He had an underdeveloped digestive system; he couldn’t even digest my breast milk.
Nevertheless, he was an attractive baby who enjoyed the comfort of familiar faces and daily routine. From birth, he benefited from lots of cuddles and love. One NICU nurse commented, “Evan is such a sweet baby and a definite snuggle bug—he nuzzles right up on my shoulder.”
The doctors supplemented Evan’s nutrition with an IV for weeks until he could finally metabolize my milk, and he was tube-fed until he was coordinated enough to breastfeed successfully.
After a few weeks in the NICU and only thirty-five weeks gestation, Evan started putting on some weight. The doctors wanted to give him his first of a series of three hepatitis B vaccines. I was concerned because he wasn’t even a full-term baby yet, but I had always been a rule follower.
A soft-spoken and even-tempered neonatal physician reassured me that the benefits of vaccinating greatly outweighed the associated risks. Up to that point, I saw the doctors as angels on earth, and I was a very trusting person. After all, it was their quick decision to take Evan out of me by emergency C-section that saved his life, and it was their miraculous work that was giving him optimal health. So, when the neonatal doctor informed me that Evan needed his first shot before he left the hospital, I consented.
Evan continued drinking breast milk, breathing on his own, and gaining weight. When he weighed 5.5 pounds, the hospital decided to discharge him and let him come home with me.
Baby Days
I was so in love with my little boy as he gazed up at me with a look that said, “I love you, Mommy.” I quickly learned within only a few days that Evan loved regular breastfeeding times, nap times, and bath times.
He loved his comfortable, cozy blankets and was a sensory-seeking baby. Like most infants, he liked to suck on a pacifier or his upper lip and seemed to need a soothing touch. However, he appeared sensitive to certain textures, tags or seams on his clothing, certain mushy foods, and loud noises. He became startled very easily. He had an aversion to bare feet on the grass and seemed to have many other sensory issues.
As a preemie, Evan started physical therapy almost immediately. The NICU sent us straight to a physiatrist at a pediatric rehabilitation center. He needed a prescription so that the insurance company would cover vigorous physical therapy. Well, that was a joke, considering it covered twenty visits per calendar year, and we needed to pay for the rest. I was thankful that Steve and I had some savings.
Evan was diagnosed with hip dysplasia due to his breech position and hypotonia (decreased muscle tone). Hip dysplasia in pediatrics/neonatal orthopedics is used to describe unstable/dislocated hips and poorly developed hipbone sockets. In addition, he had acute torticollis, a condition sometimes called “wry neck,” and a flat head. A corrective helmet was recommended by the pediatric neurologist in the NICU.
A friend recommended a local craniosacral therapist, however, who was wonderful. It was my first taste of alternative treatment that proved successful. In weeks, she was able to correct Evan’s flat head, and she resolved the torticollis within a few months.
As we started the long trek of treatment, it was recommended that Evan attend therapy sessions at least four days a week. This was the beginning of feeling that my life was no longer my own. I immediately went straight into Mommy Mode. I was lucky to be able to take five months off from my psychotherapy practice, because I felt it was my obligation to do everything I could to help my son. My own life took a backseat to his treatment, and I remember feeling increasingly alone as contact with my friends and colleagues dwindled.
As a first-time mother and the mother of a preemie, I listened to the advice of doctors and therapists who said that Evan was...
| Erscheint lt. Verlag | 23.6.2017 |
|---|---|
| Sprache | englisch |
| Themenwelt | Kunst / Musik / Theater ► Design / Innenarchitektur / Mode |
| Sachbuch/Ratgeber ► Gesundheit / Leben / Psychologie ► Familie / Erziehung | |
| ISBN-10 | 0-9904396-1-5 / 0990439615 |
| ISBN-13 | 978-0-9904396-1-5 / 9780990439615 |
| Haben Sie eine Frage zum Produkt? |
Größe: 1,4 MB
Digital Rights Management: ohne DRM
Dieses eBook enthält kein DRM oder Kopierschutz. Eine Weitergabe an Dritte ist jedoch rechtlich nicht zulässig, weil Sie beim Kauf nur die Rechte an der persönlichen Nutzung erwerben.
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen dafür die kostenlose Software Adobe Digital Editions.
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen dafür eine kostenlose App.
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich