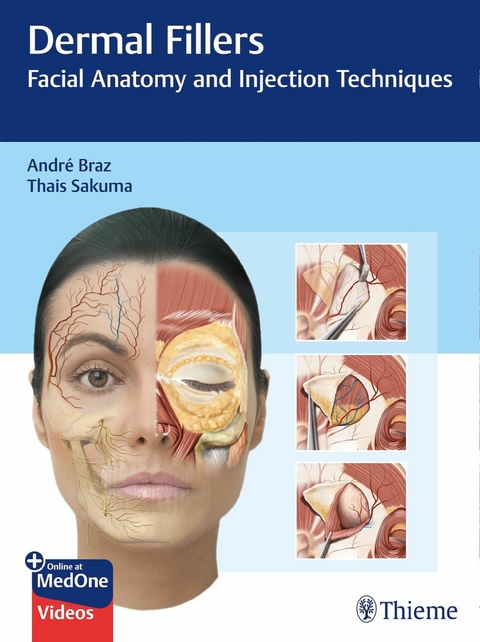
Dermal Fillers (eBook)
1021 Seiten
Thieme (Verlag)
978-3-13-258263-7 (ISBN)
| Chapter 2 | Anatomy of the Face |
Fat Pads
According to some studies, the subcutaneous tissue of the face is not homogeneous, and is divided into numerous different anatomical units called fat pads. These in turn are classified as superficial and deep (Figs. 2.1–2.13). They are separated by very thin fibrous septa that are, in fact, simply projections of the superficial muscular aponeurotic system (SMAS).a Changes in volume and position of these fat pads over the years are at least partially responsible for aging of the face: In a young face, the transition between these pads is smooth, whereas aging causes an abrupt change in the contour of these regions. Consequently, understanding this anatomy makes it possible to achieve better precision, efficacy, and safety when treating patients1,2 (Figs. 2.14–2.16).
Periorbital Fat Pads
Superficial Fat Pads
The literature describes three superficial fat pads (SFPs) around the eyes: superior, inferior, and lateral. The first two are delimited externally by the orbicularis retaining ligament and are under the skin of the upper and lower eyelids, respectively. The inferior fat pad is so thin that it cannot always be found when dissecting fresh cadavers. The top of the lateral fat pad is delimited by the inferior temporal septum and the bottom by the superior malar septum (Figs. 2.17 and 2.18).3
Deep Fat Pads
The orbit is the base of the periorbital complex and is formed by the frontal and zygomatic bones, and the maxilla. It has a cone -like structure that holds the eyeball, the intraocular muscles, and the orbital fat, which principally lubricates and cushions the eyeball and intraocular muscles. Inferior orbital fat is divided into three pads—nasal, central, and lateral—which are restrained by the orbital septum that extends from the tarsus to the inferior orbital rim. Protrusion of this fat translates clinically as “fat bags” (Figs. 2.19 and 2.20).
The palpebral portion of the orbicularis oculi muscle covers the orbital septum, and inserts distally in the inferior orbital rim. The orbital portion of this muscle originates below the palpebral portion, 0.5 to 1 cm below the inferior orbital rim. It is covered by the nasolabial and superficial medial cheek fat pads and rests laterally over the suborbicularis oculi fat (SOOF), also known as prezygomatic fat. The SOOF is didactically divided into medial and lateral portions (Figs. 2.21 and 2.22).
Retroorbicularis oculi fat (ROOF) is the fat pad located deep to the orbicularis oculi muscle, which originates medially at the level of the supraorbital nerve and extends laterally over the superior orbital rim (Figs. 2.4 and 2.19).
Fat Pads of the Middle Third of the Face
The fat in the middle third of the face includes a superficial and a deep portion. The superficial portion comprises the nasolabial, medial cheek, and middle cheek fat pads, as shown in Figs. 2.23 and 2.24. The deep portion comprises the medial and lateral cheek fat pads and the SOOF, also called prezygomatic fat (Figs. 2.21 and 2.22). The SMAS lies between the superficial and the deep portions, encompassing the levator muscles of the upper lip and ala of the nose, the upper lip, the minor and major zygomatics, and the vessels and nerves (Figs. 2.25–2.27).4
Temporolateral Fat Pad
This fat pad extends from the temporal to the cervical region. The temporal region is below the skin and above the superficial temporal fascia of the temporal muscle (Figs. 2.1–2.39).4 The upper part of this region is delimited by the temporal line (prominence of the frontal bone); the lower part is delimited by the zygomatic arch; the anterior part is delimited by the external orbital rim; and the posterior part is delimited by the scalp. The superficial temporal artery is in the posterior region of this fat pad. The distal portion covers the mandibular angle and the mandibular line, resting over the parotid gland and the mandibular body (Figs. 2.28 and 2.29).
Jowl Fat
This fat pad gives a “bulldog” appearance to the lower third of the face, and is located above the inferior rim of the mandibular body. It is delimited medially by the depressor muscle of the angle of the mouth (DMAM); the upper part is delimited by the nasolabial and medial cheek fat pads, the lower part by the platysma muscle, and the posterior part by the facial pedicle. It is divided into superficial and deep fat pads (Figs. 2.30 and 2.31).5
Fat Pad of the Lips
The lips are formed by an internal portion, the labial mucosa (nonkeratinized stratified squamous epithelium and chorion rich in blood vessels and minor or accessory salivary glands), by a transition region, the vermilion border (keratinized stratified squamous epithelium without hair follicles, apocrine or salivary glands, and possibly sebaceous glands), and by an external portion comprising the skin and its appendages. The internal portion is moist, while the others are dry. The muscle fibers of the orbicularis oris muscle insert into the border between the internal portion, the labial mucosa, and the transition area, the vermilion border. The orbicularis oris muscle delimits two compartments:
■Superficial fat pad of the lips (SFPL), posterior to the vermilion border (VB) and anterior to the orbicularis oris muscle (OOM).
■Deep fat pad of the lips (DFPL), posterior to the orbicularis oris muscle (OOM) and anterior to the labial mucosa (LM)6 (Figs. 2.32 and 2.33).
Buccal Fat Pad (Bichat’s Fat Pad)
The buccal fat pad, also called Bichat’s fat pad, was first described in 1732 by Heister, who thought this tissue had a glandular origin. However, Marie François Xavier Bichat, a French anatomist and physiologist, was the one who, in 1802, recognized it as a fat pad. Bichat’s fat pad is directly related to the chewing muscles and, in childhood, it helps in sucking and confers a cherubic look.
It is a deep fat pad in the center of the submalar triangle. It has a triangular shape, with extensions between the masseter, temporal, and pterygoid muscles, and rests over a fissure above the buccinator muscle and below the SMAS. The facial artery and vein are located anteriorly to Bichat’s fat pad. The transverse facial vessels supply to its superior portion, above the parotid duct, and branches of the internal maxillary artery also contribute to vascularization.
The parotid duct and the zygomatic and buccal branches of the facial nerve are intimately related to the buccal fat pad, as shown in Figs. 2.34 to 2.39.
Vascularization
The external carotid artery divides into an average of eight branches that supply the face and structures of the neck. These are: the superior thyroid artery, ascending pharyngeal artery, lingual artery, facial artery, occipital artery, posterior auricular artery, superficial temporal artery, and maxillary artery. The internal carotid artery does not divide into branches until it enters the cranium.
After joining the facial vein, the facial artery becomes more superficial, passes over the inferior edge of the mandible at the level of the anterior rim of the masseter, and then penetrates the face (Figs. 2.40-2.44 and Fig. 2.57). The inferior labial artery originates close to the oral commissure; it branches anteriorly under the depressor muscle of the angle of the mouth and, crossing the orbicularis oris muscle, presents a tortuous path along the edge of the lower lip, between this muscle and the mucous membrane. The inferior labial artery anastomoses with the contralateral artery. The superior labial artery is larger and its overall path is more tortuous than the inferior one; it follows the same course along the edge of the upper lip, lying between the mucous membrane and the orbicularis oris muscle, as shown in Figs. 2.40, 2.41, 2.43-2.48, 2.55, 2.56, and Figs. 2.58-2.62. The superior labial artery also anastomoses with the contralateral artery and divides into a septal branch, which supplies the nasal septum, and an alar branch, which supplies the ala of the nose. After dividing into these two branches, the facial artery continues its ascending course and divides into the lateral nasal branch. This supplies the ala and nasal dorsum, and anastomoses on the contralateral side with the septal and alar branches, the dorsal nasal branch of the ophthalmic artery, and the infraorbital branch of the maxillary artery (Figs. 2.40, 2.41, and Figs. 2.43-2.45). The angular artery is the terminal part of the facial artery (Figs. 2.40, 2.41, 2.43, 2.44, 2.45, and Figs. 2.47–2.52); it ascends in the direction of the medial angle of the orbit in the midst of the fibers of the levator muscle of the upper lip and the ala of the nose, accompanied by the angular vein more laterally. The branches of the angular artery anastomose with the infraorbital artery and then, after supplying the lacrimal sac and the orbicularis oculi muscle, anastomose with the dorsal nasal branch of the ophthalmic artery (Figs. 2.40, 2.41, 2.43, 2.44, 2.45, 2.47, 2.48–2.50, and Fig. 2.53).7
The superficial temporal artery, the smaller of the two terminal branches of the external carotid, is a continuation of this vessel. It has its origin inside...
| Erscheint lt. Verlag | 16.9.2020 |
|---|---|
| Verlagsort | Stuttgart |
| Sprache | englisch |
| Themenwelt | Medizin / Pharmazie ► Medizinische Fachgebiete ► Chirurgie |
| Medizin / Pharmazie ► Medizinische Fachgebiete ► Dermatologie | |
| Schlagworte | cannula • complications • Contouring • FACE • Facial anatomy • global filling • hyaluronic acid • Injections • injector • Needle • SAFE • technique • volume resaturation • volumizing • wrinkles and lines |
| ISBN-10 | 3-13-258263-8 / 3132582638 |
| ISBN-13 | 978-3-13-258263-7 / 9783132582637 |
| Haben Sie eine Frage zum Produkt? |
Größe: 192,9 MB
DRM: Digitales Wasserzeichen
Dieses eBook enthält ein digitales Wasserzeichen und ist damit für Sie personalisiert. Bei einer missbräuchlichen Weitergabe des eBooks an Dritte ist eine Rückverfolgung an die Quelle möglich.
Dateiformat: EPUB (Electronic Publication)
EPUB ist ein offener Standard für eBooks und eignet sich besonders zur Darstellung von Belletristik und Sachbüchern. Der Fließtext wird dynamisch an die Display- und Schriftgröße angepasst. Auch für mobile Lesegeräte ist EPUB daher gut geeignet.
Systemvoraussetzungen:
PC/Mac: Mit einem PC oder Mac können Sie dieses eBook lesen. Sie benötigen dafür die kostenlose Software Adobe Digital Editions.
eReader: Dieses eBook kann mit (fast) allen eBook-Readern gelesen werden. Mit dem amazon-Kindle ist es aber nicht kompatibel.
Smartphone/Tablet: Egal ob Apple oder Android, dieses eBook können Sie lesen. Sie benötigen dafür eine kostenlose App.
Geräteliste und zusätzliche Hinweise
Buying eBooks from abroad
For tax law reasons we can sell eBooks just within Germany and Switzerland. Regrettably we cannot fulfill eBook-orders from other countries.
aus dem Bereich